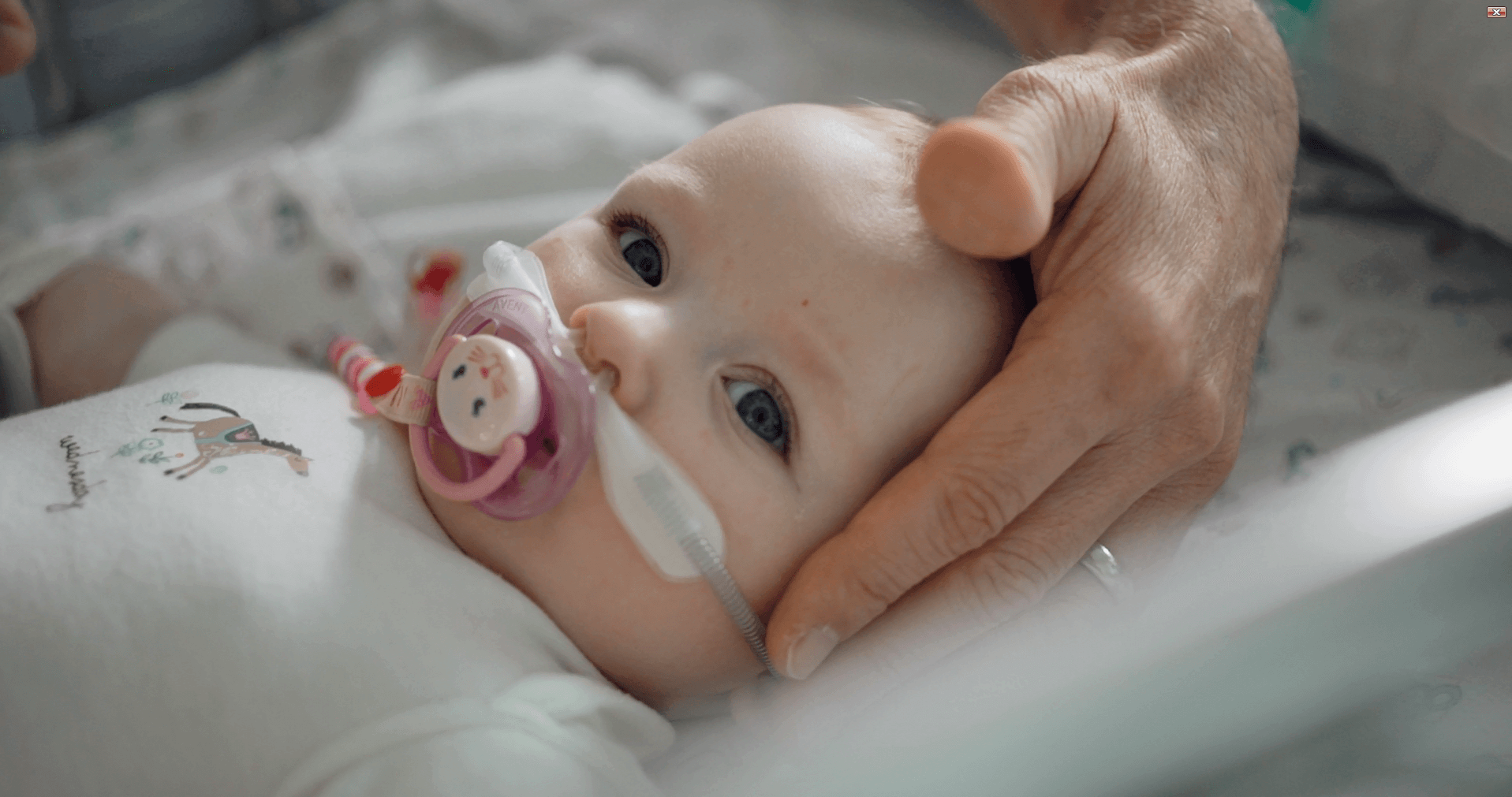
We will introduce a measured model of care using a comprehensive educational Respiratory Care Bundle for children with ARF in rural and remote hospitals in Queensland. This includes the implementation of high-flow nasal cannula therapy, which is a standard therapy used in the past decade in regional and urban hospitals in Australia but yet to be offered in rural and remote settings.
Study Outline
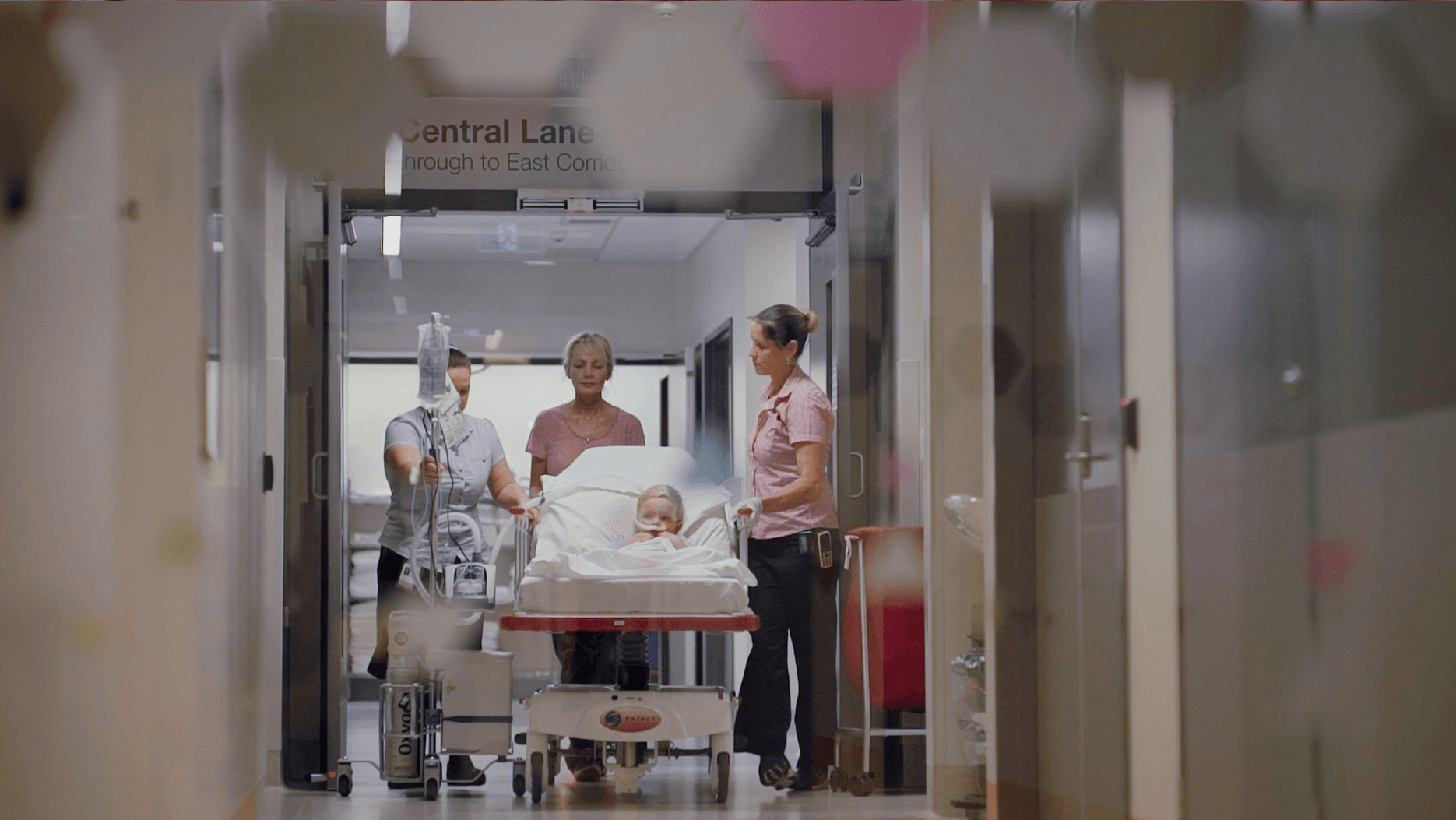
Respiratory illnesses are the most frequent reason for non-elective hospital admissions in children aged less than 5 years, with a high global health burden. Acute respiratory failure (ARF) is the common endpoint for many underlying specific diagnoses such as bronchiolitis, pre-school wheeze and pneumonia. In Australia and New Zealand, 28% of intensive care admissions for children are due to ARF. Whilst mortality due to ARF has improved in high-income countries (1-2%), mortality remains between 13-20% in less well-resourced settings.
In Far North Queensland 50%, mostly Indigenous children with ARF, require transfer to a higher level of care in a hospital either in Cairns or Townsville, whereas in South East Queensland only 9-12% of these children require inter-hospital transfer for higher level of care. This imposes significant emotional stress on families and children; and furthermore, the transfer is very expensive and perceived by many parents as unnecessary.

Respiratory Care Bundle
What does it look like? The Respiratory Care Bundle will encompass a number of clinical help tools including:
PARIS on Country webpage
With relevant links to educational resources
Face-to-face education
For all medical and nursing staff in participating remote hospital settings
Equipment
Supply High Flow equipment (Airvo3’s) and educate application and use of HFNC in children
Champion Booklets
Greater detail of children presenting with respiratory disease including:
– Paediatric physiology and changes that occur with their illness.
– Differences between adults and children
– High flow therapy use in children, including flows
– Nasogastrics and when to use with high flow patients
– Nebulisers and how best to use with high flow patients
The aim of this project
To reduce the number of transfers and offload the pressure on the emergency departments and retrieval systems in remote settings and ultimately reduce the cost on the health care system. Notably, keeping Indigenous community members in their country/community environment has not only positive psychological and social-emotional impacts, but it also has significant health care economical savings.

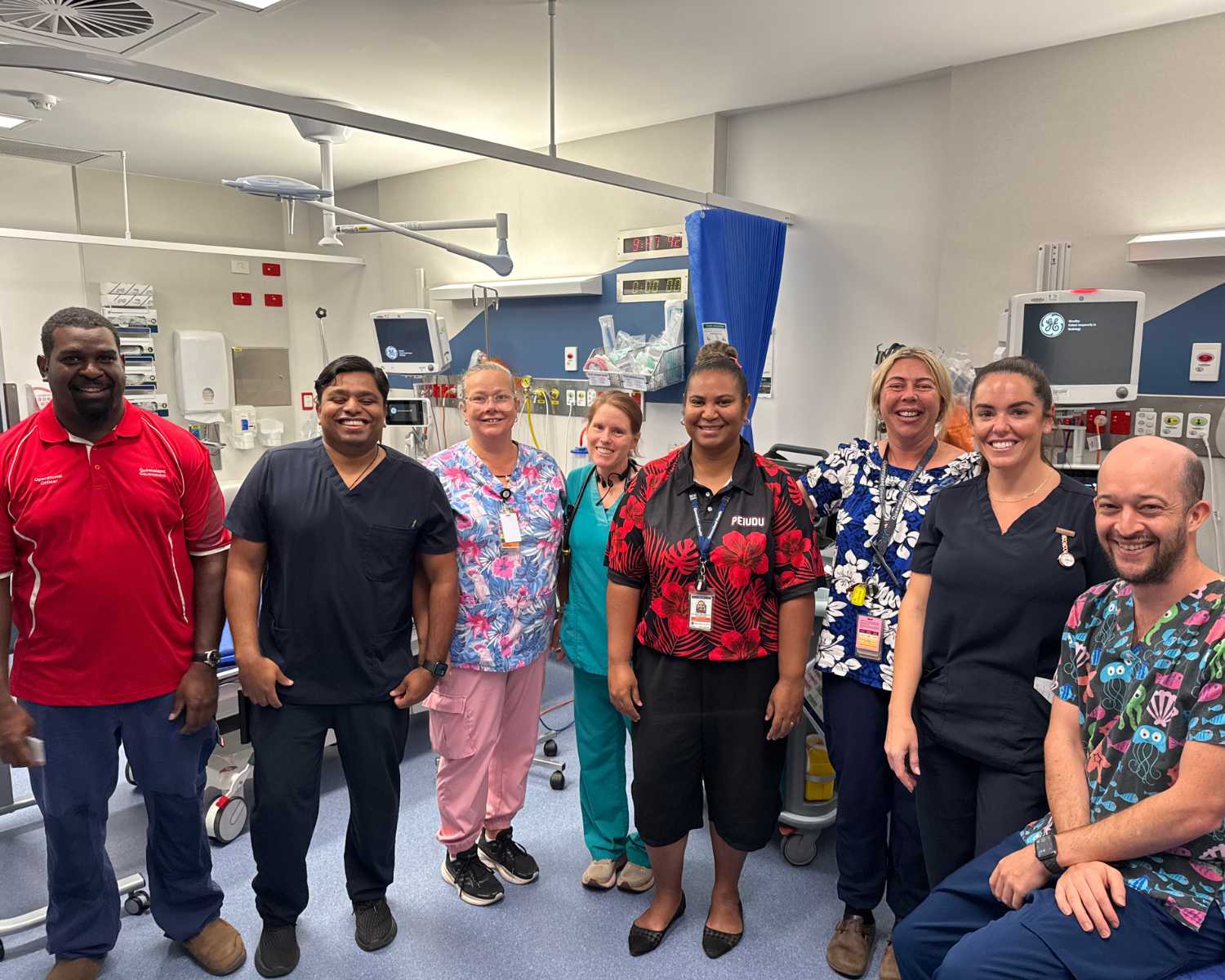
Hospitals currently implementing and live with the study
Hospital NOW LIVE with the implementation of this study as of April 2024.
- Cloncurry Hospital, NWHHS
- Cooktown Hospital, TCHHS
- Mareeba Hospital, CHHHS
-
Atherton Hospital
-
Innisfail Hospital
- Normanton Hospital
- Thursday Island Hospital
Please note that three of the 14 hospitals have been part of a pilot study for this larger project (REMOTE PARIS) and have therefore had earlier training using high flow therapy in children. These hospitals include Cooktown, Weipa and Thursday Island hospitals. Although they may not all have commenced the implementation phase for this study as yet, it is important to take their current expertise and skill level/competence into context when higher level services (Level ≥4 CSCF facilities) are advising care/management in the rural hospital setting.
Remaining sites are yet to commence the implementation phase. Each will commence once their randomisation timeframe occurs – this will be between October 2024 and October 2025 with a staggered approach.
- Tully Hospital
- Mornington Island Hospital
- Mossman Hospital
- Mt Isa Hospital
- Weipa Hospital
- Doomadgee Hospital
- Bamaga Hospital
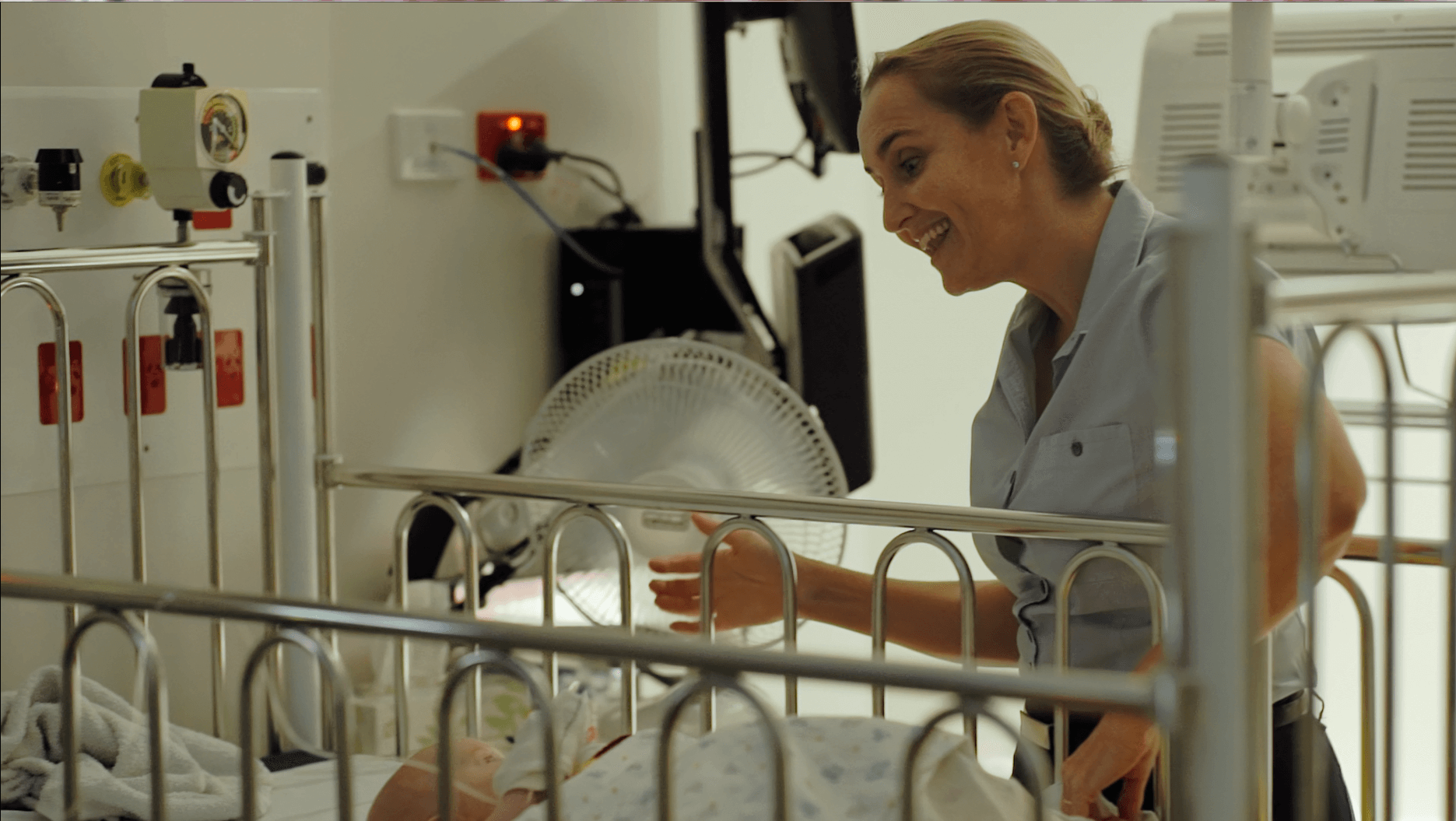
Gallery
Implementing adequate remote care
The implementation project follows a stepped wedge cluster randomised trial design where group of 3 to 4 hospitals will initiate the implementation process at six-month intervals over an 18-month period. Once all sites have successfully implemented the respiratory care bundle, the project will enter a monitoring phase. During this period, researchers actively contribute to education for an additional 6 months, providing a total of over 2 years of support for the initially clustered hospitals. Subsequently, the sites will transition to independent management.
Researchers will continue to collect data for another year to assess differences across phases – from the control phase (current management of children admitted with respiratory illnesses) to the implementation phase, where hospitals manage patients using the tools introduced during implementation without ongoing researcher support.

Online Survey
Throughout the project, staff members will be requested to participate in an online survey designed to gauge their confidence in caring for a child presenting or admitted with an acute respiratory illness. This survey will be administered every six months throughout the project’s 2.5-year duration.
Participate in Interviews
Additionally, parents of children admitted and/or transferred will be invited to participate in interviews with the researchers. These interviews aim to gather insights into socio-economic factors and the impacts on families, providing valuable information for the project.