Oxygen therapy in infants and children
Theory and Evidence behind Standard Oxygen and High Flow Nasal Cannula Therapy in Infants and Children
In both, infants and children oxygen therapy is required if the patient presents with a SpO2 reading that is consistently less than 90%. A SpO2 measurement should be performed for any infant or child presenting with breathing difficulty. The SpO2 needs to be performed on a warm and well perfused limb and a good waveform (good signal quality). If SpO2 is less than 90% then start standard oxygen therapy (SOT).
OXYGEN (including its dangers)
What is Oxygen?
Oxygen is a commonly used therapy for hypoxaemia in the management of bronchiolitis and other respiratory illness/diseases in the paediatric population.
Oxygen is a drug, which should be administered with care at all times. If Oxygen is given in a too high quantity, then Oxygen toxicity can occur, which can harm the lung, the brain and the heart. An example of how this knowledge has changed practice, is with newborns who are currently being resuscitated in room air due to the risks associated the adverse effects and toxicity of Oxygen.
The purpose of supplemental Oxygen is indicated to relieve the following:
- Hypoxaemia – inadequate supply of Oxygen in blood. (An inadequate supply of Oxygen in tissues is called Hypoxia).
- Reduce myocardial stress due to hypoxaemia that is the stress to the muscle tissue of the heart.
Signs and Symptoms of Hypoxaemia
- Confused, agitation
- Hypertension
- Tachypnoea
- Cool, clammy skin
- Tachycardia
- Dyspnoea
- Shallow and/or laboured breathing
Dangers of Oxygen include:
- Oxygen toxicity if exposure is high and prolonged
- Atelectasis (blockage of the bronchioles by mucus or by pressure on the outside of the lung, preventing normal Oxygen absorption to healthy tissues).
- Carbon dioxide retention causes respiratory drive depression
- Oxygen derived free radicals which is the end product of too much Oxygen causing cellular damage to the lungs.
Standard Oxygen Therapy
Standard oxygen therapy (SOT) is defined by using subnasal cannula up to 2 L/min of 100% oxygen or using a Hudson Face Mask using up to 8L/min. The aim of standard oxygen is to titrate the SpO2 to 90-94%. It is not necessary to achieve 100% as oxygen is a drug with side effects known as oxygen toxicity, which can harm the patient if excessively used.
In infants with Bronchiolitis (aged < 1 year) with an oxygen requirement on SOT:
Escalation of respiratory support from SOT to High Flow Nasal Cannula (HFNC) therapy should be considered if one or more of the following is present within the first 2 hours of SOT applied:
- Oxygen saturation cannot be maintained SpO2 ≥90% with SOT (2L/min subnasal)
- Heart Rate remains unchanged since SOT commenced
- Respiratory rate remains unchanged since SOT commenced
- Work of breathing and recession remain unchanged since SOT commenced
In children (aged 1-4 years) with acute respiratory failure (breathing problems and oxygen requirement) on SOT:
Escalation of respiratory support from SOT to HFNC therapy should be considered if one or more of the following is present:
- heart rate remains >160/min for longer than 2 hours since SOT commenced
- respiratory rate remains >45/min for longer than 2 hours since SOT commenced
- oxygen requirement on SOT exceeds standard oxygen therapy (2 L/min by nasal cannula, or 8L/min by face mask) to maintain SpO2 ≥90%
- the hospital internal Early Warning Tool (CEWT) calls for medical review since SOT commenced
- increased work of breathing requiring escalation of respiratory support and assessed as moderate to severe respiratory failure.
Oxygen Therapy Flow Chart
HFNC Therapy
High Flow Nasal Cannula (HFNC) therapy
High Flow Nasal Cannula therapy is a form of non-invasive respiratory support consisting of three components (Diagram 1).
The oxygen in conjunction with air and humidification is delivered to a patient at rates of flow higher than that delivered traditionally in oxygen therapy.
Traditional oxygen therapy is up to 8 L/min in children via Hudson mask (sometimes higher) and HFNC therapy is up to 50 L/min in children. Adults will have flows up to 60L/min.
HFNC therapy is delivered using a device through the integration of heated humidification and gas delivered via nasal cannula adapted to a child’s nares size (Diagram 1). It can be delivered with or without increased fractional oxygen. Some children manage well on HFNC therapy in room air alone (21% FiO2). HFNC therapy is a method for providing oxygen and continuous positive airway pressure (CPAP) to children with respiratory distress. It provides positive airway pressure at levels similar to those provided by CPAP. The positive pharyngeal pressure can significantly reduce the work of breathing and improve gas exchange.
The higher flows administered with HFNC therapy has been associated with improvement in washout of nasopharyngeal dead space, lung mucociliary clearance, and oxygen delivery compared with other oxygen delivery systems. HFNC therapy creates a reservoir with high FiO2 in the nasal cavity when needed. HFNC therapy is a continuous flow of gas that is able to supply the patient’s resting minute volume and reduce the work of breathing for the patient. The inspired Oxygen concentration can be titrated to the patient’s needs.
Importance of humidification and heating
Since the inspired gas is humidified and heated, there is less stress to the mucosa. It is important to note that the nasopharynx is a very effective structure in the human body, which can effectively heat and humidify itself; however, with very high flows using HFNC therapy, this can dry the mucosa out if no humidification is used. HFNC therapy can washout the dead space to allow for improved CO2 clearance.
The use of heated humidification with HFNC therapy has many positive effects, including the humidified warm gas that keeps mucous more fluid and aids airway recovery (eg, post extubation). It can optimise mucociliary clearance and the warm humidified constant flow improves gas exchange and reduces work of breathing.
Other benefits of HFNC therapy include:
- Simple and easy device to set up and use
- Improved patient comfort and tolerance
- Greater therapy success than with face masks (particularly infants)
- Improved lung volumes
- Improved physiological parameters ie. HR, RR, WOB
- Improved oxygenation with fewer desaturations
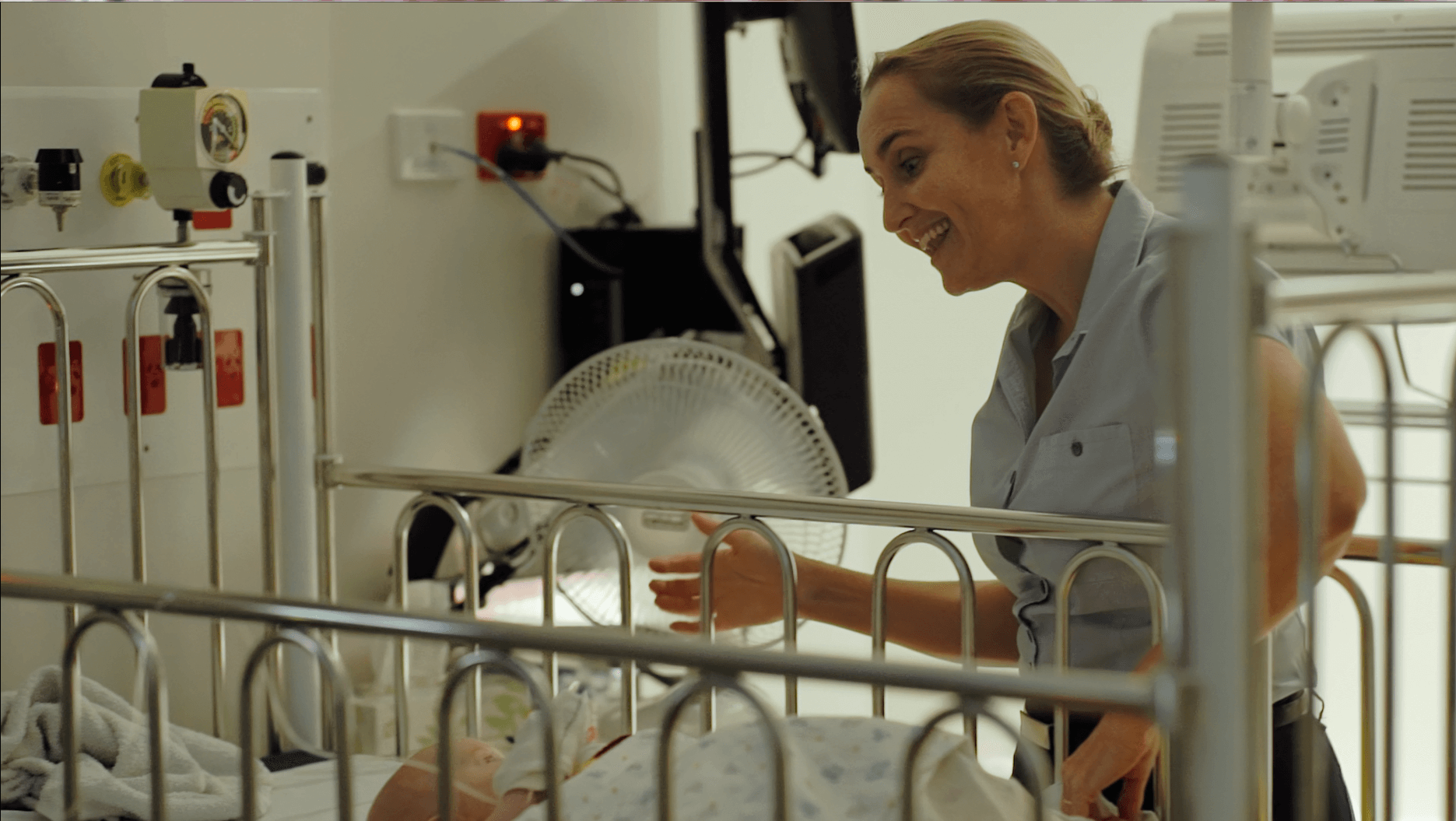
- Parental involvement is simpler ie. cuddles, bathing
- Nasal Cannula are softer and less trauma on nares
- Ability to use a battery for moving the patient from one area to another without stopping HFNC therapy
- Quick and simple cleaning/disinfection of device in readiness for next patient.
HFNC therapy use in children - WHO, WHY, WHEN and HOW
When do we use HFNC therapy?
Neonates
- Use as post extubation support – good evidence based fif used in premature infants ≥28 weeks (primarily after neonatal RDS).
Paediatrics
- In Emergency departments at the earliest presentation to aid in reducing progression of the disease process.
- Most commonly used in the bronchiolitis population in general paediatric wards – reduces LOS and reduces clinical deterioration and ICU admission
- Equally effective as CPAP in ICU preventing intubation.
- Post cardiac surgery extubation – reduces need for reintubation
- Acute hypoxaemic respiratory failure group such as asthma, pneumonia, pneumonitis, reactive airways disease to name a few.
Adults
- Post extubation cardiac surgery
- Post extubation ARDS (instead of using Mask CPAP)
- Prevents intubation in ARDS and reduces mortality
HFNC therapy flows applied in Paediatrics
HFNC therapy and the flows applied to infants and children has evolved from what we know in neonates.
- Healthy infants require 0.8 L/kg/min to match its maximal inspiratory flow.
- Chronic Lung Disease infants require 1 to 1.2 L/kg/min to match its maximal inspiratory flow.
- A sick infant requires 1 to 1.6 L/kg/min to match its maximal inspiratory flow.
Therefore, for the paediatric population of infants we have used the formula of 2L/kg/min which would average out to meet most infants needs. This is for the less than 12 month age group (for those children up to 10-12 kg in weight). (Please refer to Differences in tidal breathing between infants with chronic lung diseases healthy controls, Schmalisch, BMC, Pediatrics, 2005).
Diagram 2, below shows the inspiratory and expiratory flow of a healthy infant and the HFNC adjusted to the maximal inspiratory flow so this is nicely matched. During the inspiration phase the patient feels a push of air into the lungs and this will offload the work of breathing of the diaphragm.
Diagram 3 below shows the inspiratory and expiratory flow of a child in respiratory distress. If the HFNC flow rate is not adapted to the demand during the inspiratory phase, the infant has to entrain air around the nasal cannula, hence will only breath partially from the HFNC therapy. Therefore, the flow rate needs to be adapted to the inspiratory demand of the patient (Diagram 3). The flow rates proposed in this study should match the demand of most of the infants and children we see in respiratory distress whilst in the paediatric ward or ED. However, some may need even more flow and these infants/children are the patients that are more likely to require PICU admission.
Physiological changes with HFNC
Heart and Respiratory Rate
If the HFNC therapy is applied and the patient is responding, we can expect that the heart rate and the respiratory rate will drop. Our own data has shown that the heart rate will drop approximately by 15 beats and the respiratory rate by 5-10 breaths per minute (approximately 10-20%). This change is normally observed within the first 1 to 3 hours after commencement of HFNC therapy. If there is no change in HR and RR, it is likely that the infant is a non-responder, i.e. that this patient is likely to need higher level of care in an HDU or PICU.
Diagram 4 below shows the change of HR and RR in over 250 infants (Reduced intubation rates for infants after introduction of high-flow nasal prong oxygen delivery, Schibler et al, 2011). The open circles are the responders and the closed triangles the non-responders.
Work of Breathing (WOB)
When we breathe in and out at rest, the speed of airflow is less than if we were running/jogging. With exercise, we would suck more air in at a faster rate as the airflow requirement is greater. This is the same in the sicker child who will suck more air in and out as the lungs are sicker with alveoli that are closed with mucous plugs.
As all children have a different lung and body size, it is more convenient to describe the airflow used in L/kg/minute and not in absolute L/min. In the adult world, this difference is not usually made and absolute numbers are considered whereas in children due to the differing size a more accurate definition of the inspiratory flow needs to be made (it is similar to medication in that you administer per kilogram).
Research has demonstrated that in a healthy child the maximal air flow required with each breath inspired and expired is 0.8 L/kg/min (as mentioned earlier). For a 10kg child, this would be 8L/min needed in a healthy child. If we deliver more than this flow, we will start supporting the lung and we will reduce the work of breathing.
In a sick child who is being administered with 2L/min of subnasal Oxygen this is not enough air flow to reduce the work of breathing. The child will be trying to entrap the air around the nasal prongs from the atmosphere to meet the require 8L/min or more for a 10kg child. If the child is sick then 8L/min would not even meet the requirement to match their inspiratory air flow with each breath.
This is where the 2L/kg/min or the adapted flow rates for older children in our HFNC flow rates Table (Table 1) is required to ensure more air flow into the lungs to reduce the work of breathing and allow the alveoli to open up and provide better ventilation. Therefore, this explains why increasing Oxygen does not reduce the work of breathing, but adequate high flow does.
Work of breathing and Oxygen saturations are two different variables and the flow of air is what will open the alveoli and reduce the work of breathing rather than Oxygenation.
Tolerance/limitation
This study is also investigating the tolerance level of HFNC therapy and standard oxygen therapy. It is therefore important to document how your patient copes with the application of the nasal cannula and the flows given in the nursing and medical notes.
Nebuliser during SOT and HFNC therapy
On SOT Therapy
If using a MDI, the drugs can be delivered by placing the mask over the nasal cannula. If you are not able to achieve a good seal with SOT in place when administering medication with a MDI, then you will have to remove the nasal cannula and administer the medication via the MDI and then return the patient to SOT and previous settings used.
If you use a nebuliser which doesn’t have a seal this can be used by leaving the nasal cannula in place.
On HFNC Therapy:
During administration of the nebuliser/MDI reduce the flow down to 2L/min (infants/children ≤12kg) or 10L/min (Children >12kg). Do this by decreasing flow using the AIRVO up and down arrows. Then increase to FiO2 to 95% (AIRVO2) or 100% (AIRVO3). The AIRVO2 will alarm at 100% and the AIRVO3 will not. Observe the machine display screen for FiO2 value. Administer nebuliser or MDI.
Following the nebuliser/MDI completion, return patient to previous AIRVO settings, changing both the L/min flow and reducing the FiO2 to the previous settings – observe the machine display screen.
If you are not able to achieve a good seal with HFNC therapy in place when administering medication with a MDI, then you will have to remove the nasal cannula and administer the medication via the MDI and then return the patient to HFNC therapy and previous settings used.
Nutrition and HFNC
For all acute hypoxaemic respiratory failure patients, regardless of SOT or HFNC, feeding and fluid management should occur according to standard hospital practice.
At this point in time there is no clear evidence that suggests it is safe to give oral feeds to children on HFNC therapy. There is no research that has demonstrated its safety in children, so for this study please follow the below guide.
For all patients on HFNC therapy, a nasogastric tube (NGT) is encouraged in the 2-3 year age group however, it is at the discretion of the attending clinician. If a NGT is inserted, position confirmation is mandatory as per local practice (x-ray, pH).
The insertion of a NGT tube is not mandatory and good clinical judgment should prevail.
Regular de-venting of the stomach through aspiration of the NGT needs to be performed every 4 hrs (minimum). With regards to oral feeding when on high flow, there is a potential risk of aspiration. When a child wants to eat or drink orally, please reduce the flows for a maximum of 20 mins at the following flows and then return them to their previous high flow settings.
NB: The Airvo2 and Airvo 3 have different mode settings whereby Airvo2 in Junior mode will only allow flows to a certain delivery.
Airvo 2 – Junior and Adults(default) mode settings (Junior mode up to 25L/min only)
Airvo 3 – no different modes and can alter flows as required.
Refer to the table below for specifics.
Nursing acuity
Nursing ratio should be provided as per standard practice in your hospital and current skill mix. It is imperative that the nursing ratio is not increased because of the patient on HFNC therapy. It is very important to note that all study patients, whether they are on SOT or HFNC, are staffed as per current hospital practice for all patients requiring regular Oxygen therapy.
HFNC patients do not require a higher nurse/patient ratio just because they are on HFNC therapy. When looking at allocating staff to these patients it is important to look at each patient requiring an Oxygen requirement, rather than on HFNC therapy. If you normally staff a patient with a higher Oxygen requirement and greater nursing care and observation frequency on a smaller nurse/patient ratio, then continue this practice, however if the patient is on less Oxygen requirement and less nursing care is required, then staff accordingly. The majority of these patients will be a 1:4 ratio as the study is only changing the way in which Oxygen therapy is provided to these children. A patient who is admitted to your ward on HFNC therapy does not necessarily demand greater nursing care than a patient admitted on standard oxygen therapy.
Both patient types require observations at the same time, both require basic care including but not limited to suctioning of the nares, nappy changing, bathing etc. The only difference is one is being provided with Oxygen via nasal cannula at a low flow (via wall Oxygen) and one is being provided Oxygen via nasal cannula at a high flow (via a simple machine).
This outlines that there is really very little difference in the care of children on standard oxygen therapy or HFNC therapy and the nurse/patient acuity should reflect this. HFNC therapy patients do not demand higher nurse/patient ratios unless they have deteriorated and require escalation in their care.