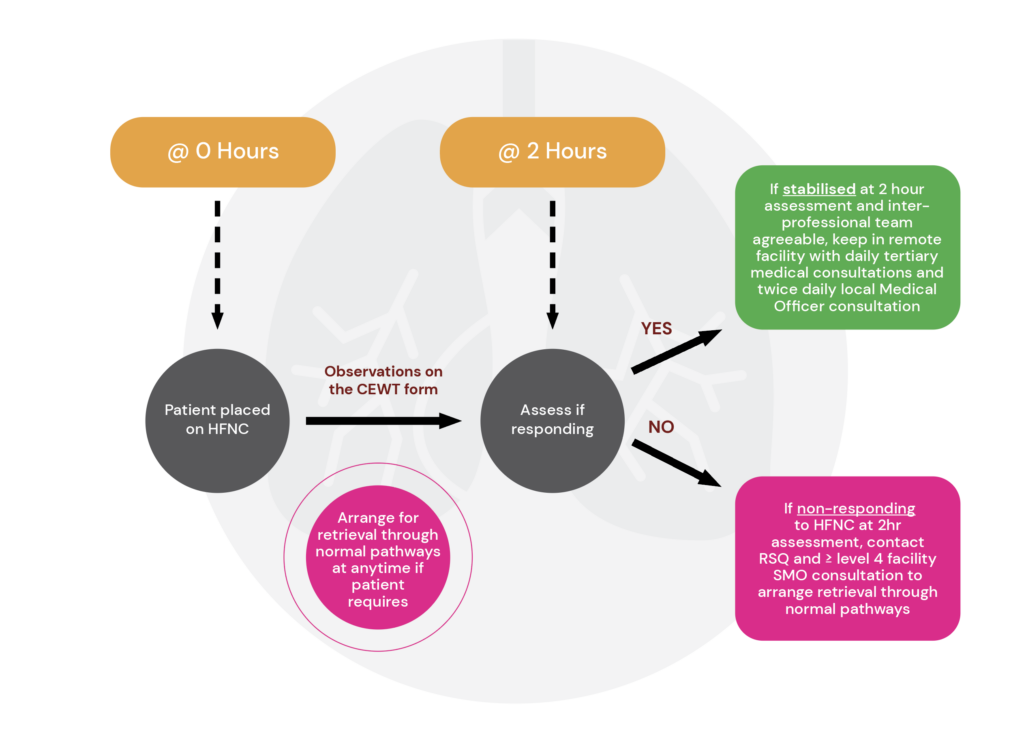
Referring clinicians to contact their relevant level ≥4 CSCF facility for consultation – this should be Senior Medical Officer (SMO) level referral at both facilities.
If retrieval is required in the first instance contact RSQ (1 300 799 127) to link all relevant parties together including:
- referring SMO from a remote hospital
- local level ≥4 CSCF facility
- relevant local Intensive Care Specialist – dependent on the patient’s condition